General SurgeryRectal Cancer
Treatment of Rectal Cancer – General Outline
The surgical treatment of rectal cancer is technically more challenging than colon cancer because rectum is located within the bony confinement of pelvis. Because of gender difference, the male pelvis is always more challenging than the female ones.
For mid and lower rectal cancer (clinically referring to lesions located within 10cm from anal verge), the standard surgical treatment is total mesorectal excision (TME). In order to achieve a good quality TME specimen, surgical resection needs to follow an avascular anatomical plane between the presacral and the mesorectal fascia. Vessels, lymphatics and lymph nodes around the rectum are all enveloped by the mesorectal fascia.
TME specimen
Adequate margins have to be achieved so as to reduce the chance of local recurrence. Proximal margin is never a concern. However, distal and circumferential resection margins must be carefully assessed before the operation, which involves clinical, endoscopic and radiological assessment. Among these 3 modalities, MRI pelvis is the most important one, as it can objectively estimate the distal and circumferential resection margin that one can achieve. Moreover, it can provide valuable information about the relationship of the rectal tumour with adjacent organs, the presence of suspicious lymph nodes (nodes likely to harbour malignant cells) and the presence of extramural venous invasion.
The rectal cancer invaded to uterus
Circumferential resection margin
threatened by suspicious lymph node
Neoadjuvant treatment needs to be considered
Sphincter preservation is always the top priority concern for patients having lower rectal cancer (lesions within 5cm from anal verge). In reality, how much distal margin is considered safe? 2cm distal margin for lower rectal cancer is often considered adequate. Sometimes 1cm distal margin is adequate for cancers without adverse histological features.
Nonetheless, circumferential resection margin (CRM) is important as the amount of CRM significantly influences future local recurrence rate even if a high quality total mesorectal excision been achieved. CRM is defined as the shortest distance between the rectal tumour (including non-contiguous tumour like lymph nodes harbouring tumour) and the mesorectal fascia. How much CRM is considered safe? Ideally, the more the better, though >2mm is usually adequate.
During preoperative assessment, if MRI pelvis shows threatened margin or other adverse features, then upfront surgical resection will not be advised. In order to improve the long-term treatment outcome, neoadjuvant treatment (e.g. long course chemoradiotherapy) would be considered, which aims to down-stage the tumour. Upon completion of neoadjuvant treatment, apart from clinical and endoscopic assessment, restaging imaging will be performed to evaluate the treatment response. Definitive surgery can usually be performed in 8-12 weeks after the last dose of radiotherapy.
Nowadays minimally invasive surgery is the preferred approach for rectal cancer surgery. Laparoscopic rectal cancer resection has been accepted as a standard of care for suitably selected patients.
Anastomosis performed under laparoscopic guidance
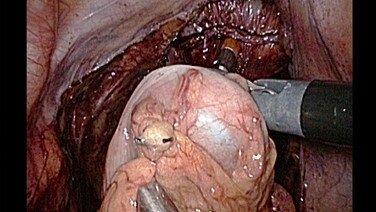
Despite technological advancement over the past decade, like visual system and stapling devices, laparoscopic total mesorectal excision remains technically challenging for some individuals. This is especially true for male pelvis with enlarged prostate or females with uterine fibroids. High BMI is also another well-known factor, which increases the difficulties encountered during Laparoscopic total mesorectal excision. All the above-mentioned factors make the dissection deep down in the pelvis difficult, as the volume of the pelvis is getting smaller and smaller when the dissection proceeds downward towards the pelvis floor.
Narrow pelvis of male patient
A large uterine fibroid in a rectal cancer patient
Patient with high BMI
Transanal total mesorectal excision is one of the key developments in rectal cancer surgery over the past decade throughout the world. Basically, this is a bottom-up approach when compared to the conventional method. A special anal platform, which simulates a single laparoscopic port, is inserted in the anal canal, through which a purse string suture is placed below the tumour to close the rectal tube. With the aid of carbon dioxide insufflation through the anal platform and under the guidance of 3D laparoscope, full thickness incision is made at the determined distal margin. The surgeon will then follow the correct anatomical plane, working from below upward. This helps to overcome some of the technical difficulties encountered in the narrow lower pelvis and a more defined distal margin can be assured.
Set up for transanal total mesorectal excision
For sphincter preserving total mesorectal excision with primary anastomosis, a temporary diversion stoma is often needed to minimize the severity of pelvic sepsis in case of anastomotic dehiscence. Either loop ileostomy (from terminal ileum) or loop colostomy (from proximal transverse colon) can be fashioned for faecal diversion. These stomas can be closed when all the adjuvant treatment or when the anastomosis healing has completed.
Loop ileostomy
Despite restoring GI continuity, about 70% patients experience various degree of bowel dysfunction after rectal resection, this is especially true in the first few months after surgery. Frequent bowel movements, clustering of motions, urgency and incontinence of flatus / liquid stool may occur. Bowel function will usually improve after a period of adaptation, with the aid of dietary modification and sometimes medication.
The above are just general information outlining the treatment pathway of rectal cancer. Patients should seek advice from colorectal surgeons or oncologists, to have a better understanding of their disease before making the most appropriate treatment plan.
Know More
 View Profile
View Profile View Profile
View Profile View Profile
View Profile











 Booking:
Booking: 
 Specialist Outpatient Centre, 1/F, CUHKMC
Specialist Outpatient Centre, 1/F, CUHKMC