Weight Management and Metabolic Surgery Clinic
Service Hours
MON - FRI: 9:00AM - 5:00PM
SAT: 9:00AM - 1:00PM
SUN AND PUBLIC HOLIDAYS: CLOSED
Contact Us



Introduction
This clinic upholds the concept of healthy weight control, provides integrated and comprehensive weight loss treatment through a multidisciplinary approach. Personalised and all-round weight loss plan is offered for people with different degree of obesity to achieve effective weight control.
Our Services
Your Weight Management Plan
- Fundamental Weight Management - Dietary & Physical Training Programme
- Advance Dietetic & Pharmacological Treatment
- Metabolic & Bariatric Surgical Programme
- Intragastric Balloon Programme
- Endoscopic Sleeve Gastroplasty Programme
To maximise treatment outcome, advanced therapeutic technology is applied.
- MenCare/WomenCare Health Check Programme
- Metabolic and Diabetic Complication Screening
- Sleep Health Programme
- Gut Health Programme
- Heart Health Programme
- Weight Management Programme
Am I suitable for Metabolic & Bariatric Surgery?
When your body mass index (BMI) exceeds 30kg/m2, but conservative treatments such as diet, exercise, and medication are not effective, and chronic diseases such as hypertension, diabetes, and obstructive sleep apnea could not be controlled, it is the time for you to consider undergoing surgery to treat severe obesity. The aim of surgical treatment is to change the structure of the digestive tract and adjust the amount of food intake, so as to manage your weight and modify your dietary habit and lifestyle.
|
Introduction on Bariatric & Metabolic Suregry
- Metabolic & Bariatric Surgical programme
Laparoscopic Sleeve Gastrectomy
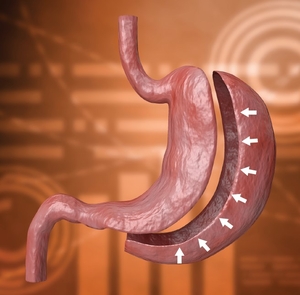
"Sleeve gastrectomy" or "vertical gastrectomy" is a new form of bariatric procedure in weight management. It involves the removal of part of the stomach and leaving a small gastric tube. This leads to a decrease in the stomach size, an increase in the patient’s sensation of fullness, and eventually causing a decrease in appetite. Furthermore, the surgery removes the secretion site of appetite-stimulating hormones and therefore increases satiety. Gastric-reflux may occur after this surgery and long-term medications may be needed. Before deciding to receive this irreversible surgery, patients should have a thorough understanding of the procedures and potential risks.
Laparoscopic Gastric Bypass
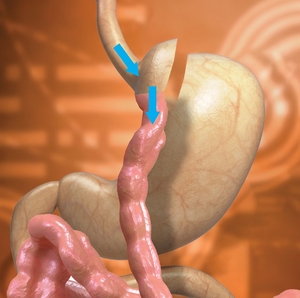
In the gastric bypass surgery, the stomach is divided into a small upper pouch and a much larger, lower "remnant" pouch. The volume of small pouch is only 20-50ml. The small intestine is re-arranged to allow food to enter distal small bowel without passage of the remnant stomach, duodenum and proximal jejunum (150-200cm of small intestine in total). Since the size of the stomach is reduced, the eating portion becomes smaller and the absorption area in the small intestine is shortened; thus, rapid weight loss is expected. The advantages of this surgery include provision of a faster weight loss and a lower chance of weight regain. This surgery also effectively treats type 2 diabetes. Most of the people with diabetes have significant improvement after surgery, and some of them may be able to wean off their diabetes medication altogether. However, patients will require to take nutritional supplements every day after surgery to prevent development of problems related to reduce absorption of vitamin and minerals after surgery, such as iron-deficiency anaemia, osteoporosis or other problems of nutrition deficiency.
Laparoscopic Adjustable Gastric Banding
The adjustable gastric band is made of soft silicone. It is adjusted by injecting saline into the port. The size of the band depends on the weight management plan and is tailor-made for patients. The band is positioned around the upper part of the stomach, forming a small pouch. It can help reduce the amount of food that a person wants to eat by inducing a sense of fullness after eating only a small amount of food. Although the weight reduction effect is less than that of gastric bypass or gastrectomy, it is relatively safe compared with other bariatric procedures. One of the drawbacks of this type of surgery is that the band will stay inside the body of the person permanently. Although this surgery helps reduce food intake, if the person continuous to consume energy-dense foods such as sugary drinks, ice cream, chocolate, etc., the expected amount of weight loss cannot be achieved.
All the above surgical procedures require general anaesthesia, and since the surgery involves removal of part of the stomach and/or joining of different parts of nowel, there is a potential risk of leakage and bleeding. Patients should have a thorough understanding of the procedures and understand the potential risks before the decision of receiving surgery.
- Non-surgical / Endoscopic Bariatric Therapy
Intragastric Balloon Programme

The intragastric balloon is inserted through the mouth and down the oesophagus into the stomach, occupying 400-600ml of space, giving a sensation of satiety. The first intragastric balloon was introduced in Hong Kong in 2006 which required the use of endoscope. The intragastric balloon is not a permanent treatment with a maximal treatment period of 6-12 months. Stomach ulcers may occur if the balloon remains in the stomach for too long. Balloon deflation may lead to bowel obstruction. After 6-12 months, the balloon needs to be removed in the same way that it was placed, via an enodscope.
Our clinic also introduce a new intragastric balloon technology, in which patient only need to swallow a “Balloon Pill”, and when the pill reach the stomach, the doctor will inflat and place the balloon in the stomach without the needs of endoscope. In about 16 weeks later, when the valve of this new balloon dissolve, it will then leave the stomach and pass out spontaneously and no need endoscopic removal. After the balloon is inserted, the body weight is expected to drop by around 10% of total body weight on average.
Patients need to aware that upon removal of the balloon, weight regain may occurs. Therefore, adherence to a healthier lifestyle such a balanced diet and regular exercise is necessary in order to avoid weight regain after this procedure. Not all patients are suitable for this procedure. Contraindications include people who have stomach ulcers, hiatus hernia and previous stomach operation.
Endoscopic Sleeve Gastroplasty Programme
Endoscopic Sleeve Gastroplasty is a endoscopic techniques to create large pleats in the stomach. We use an endoscopic suturing device to reduce the size of your stomach. This procedure does not involve the removal of stomach while still restricting the amount of food that the stomach can hold.
Download
Health Knowledge
View AllMedical Team
View AllCUHKMC Medical Team

 View Profile
View Profile- Consultant
- Specialist in Endocrinology, Diabetes & Metabolism
Clinical Associate Professor (honorary), Department of Medicine and Therapeutics, Faculty of Medicine, CUHK
 View Profile
View Profile- Consultant
- Specialist in General Surgery
Clinical Associate Professor (honorary), Department of Surgery, Faculty of Medicine, CUHK
 View Profile
View Profile- Clinical Director of Anaesthesiology
- Specialist in Anaesthesiology
CUHKMC Allied Health Team
Service Hours
MON - FRI: 9:00AM - 5:00PM
SAT: 9:00AM - 1:00PM
SUN AND PUBLIC HOLIDAYS: CLOSED
Contact Us