Obstetrics and Gynaecology
Introduction
Employing advanced medical technology, our professional team of professors, specialists, midwives, nursing and allied health staff are dedicated to providing comprehensive and caring services to women with gynaecological and obstetric needs
Service Scope
Our Centres and Clinics
| Obstetric service | General gynaecology service |
|---|---|
We provide holistic care to expectant mothers from their early pregnancy to postpartum period. There is now good evidence on the importance of the first 1000 days of life (i.e. 9 months period of pregnancy and the first 2 years of life) to the children’s long term health. We also provide pre-conception care and counselling to optimize the physical and mental health prior to pregnancy, in particular for women with underlying medical problems or previous obstetric complications. Prenatal care
Labour and delivery
Postnatal care
Post hospital discharge care
Special management
| We provide educational advice to women at reproductive and menopausal age on their wellness and care for benign gynaecological condition
|
| Gynae-oncology service |
|---|
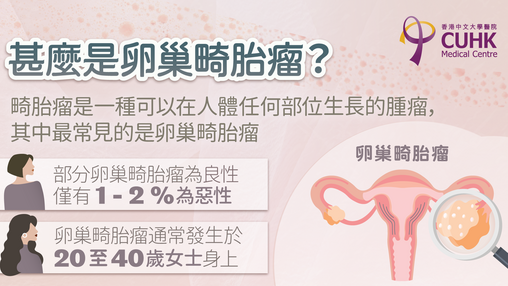
We provide the state of art services in the treatment of gynaecological caner. We work with radiotherapist and medical oncologist to offer multidisciplinary management to optimize the cancer care.
|
Fees & Packages
Feature Articles
View AllHealth Knowledge
View AllMedical Team
View AllCUHK Professorial Team

Prof LEUNG Tak Yeung
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Professor, Department of Obstetrics & Gynaecology, Faculty of Medicine, CUHK

Prof POON Chiu Yee, Liona
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Professor, Department of Obstetrics and Gynaecology, Faculty of Medicine, CUHK

Dr CHUNG Pui Wah, Jacqueline
View Profile- Consultant
- Specialist in Obstetrics and Gynaecology
Associate Professor, Department of Obstetrics and Gynaecology, Faculty of Medicine, CUHK
CUHKMC Medical Team

 View Profile
View Profile- Clinical Director of Obstetrics & Gynaecology
- Specialist in Obstetrics and Gynaecology
Clinical Professor (honorary), Department of Obstetrics & Gynaecology, Faculty of Medicine, CUHK
 View Profile
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Clinical Assistant Professor (honorary), Department of Obstetrics and Gynaecology, Faculty of Medicine, CUHK
 View Profile
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Clinical Assistant Professor (honorary), Department of Obstetrics and Gynaecology, Faculty of Medicine, CUHK
Honorary Clinical Assistant Professor, Department of Obstetrics and Gynaecology, LKS Faculty of Medicine, HKU
 View Profile
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Clinical Associate Professor (honorary), Department of Obstetrics & Gynaecology, Faculty of Medicine, CUHK

Dr CHAN Ying Tze, Viola
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology
Clinical Associate Professor (honorary), Department of Obstetrics and Gynaecology, Faculty of Medicine, CUHK
Honorary Clinical Assistant Professor, Department of Obstetrics and Gynaecology, LKS Faculty of Medicine, HKU

Dr CHEUNG Chi, Peter
View Profile- Consultant
- Specialist in Obstetrics and Gynaecology

Dr FAN Hiu Lan, Queenie
View Profile- Consultant
- Specialist in Obstetrics and Gynaecology

Dr LEE Man Hin, Menelik
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology

Dr SUEN Sik Hung, Stephen
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology

Dr TANG Sui Man, Janet
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology

Dr YAU Pui Kei, Stephanie
View Profile- Consultant
- Specialist in Obstetrics & Gynaecology