Health Check Items - Esophagus and Stomach
Esophagus and Stomach
An upper gastrointestinal endoscope is a flexible fiber-optic which consists of a camera that can view the image of the oesophagus, stomach and duodenum.
If anyone who encounter one of the colorectal cancer symptoms such as peptic ulcer disease or bleeding, black stool, stomach pain, oesophageal or gastric cancer, symptoms of indigestion, acid reflux or difficulty in swallowing, they should go for upper gastrointestinal endoscopy to check whether there is any abnormality such as ulcer or cancer.
Prior to upper gastrointestinal endoscopy, a period of 6-hour fasting is needed. Patient should inform the medical staff of any major medical problems including diabetes, hypertension and pregnancy, and continue their medications as instructed. Patient should also provide information concerning the current medications used and any allergic history. Patients should avoid driving to attend the out-patient procedure appointment and also avoid heavy drinking, smoking or use of sedative before the procedure. All patients are recommended to be accompanied by family member or friend for their safety.
Prior to the examination, local anaesthetics would be sprayed to the throat of patient. A flexible colonoscope with a diameter of 0.9-1.2 cm will then be introduced by the endoscopist through the mouth to perform the examination. In general, the procedure would last for around 15 to 30 minutes. But according to complexity, the procedure time may be prolonged.
During the upper gastrointestinal endoscopy, minor discomfort including nausea and distention discomfort of stomach is common. The local anaesthetics would keep the throat numb for approximately one hour which will lead to swallowing difficulty. Major complications including perforation, bleeding, cardiopulmonary complication, infection or acute intestinal obstruction may happen. In general, the complication risk is less than 1% but it varies depending on patients’ conditions. Complication rate would be higher in cases that require polypectomy, endoscopic hemostasis or other relevant procedures. When major complications arise, emergency surgical treatment may be needed and mortality may happen. Patient should consult the attending physician for more information before the endoscopic procedure.
Patients should remain fasted until anaethesia has worn off which will last for approximately one hour. This prevents choking with food or fluid intake. If intravenous sedation is used, patients should avoid operating heavy machinery, driving or sign any contract for the rest of the day. On the other hand, if there is any abnormality or enquiry about the examination, patient should contact our centre during office hour for query. If there is severe abdominal pain or gastrointestinal bleeding, patient should go to the nearest “Accident and Emergency” immediately and to inform their staff that upper gastrointestinal endoscopy has been done.
Related Information:
General Enquiry
Stomach Cancer
Acute upper gastrointestinal bleeding
Peptic Ulcer
Gastroesophageal reflux disease
Helicobacter pylori Infection
Functional Dyspepsia
Endoscopic ultrasound (EUS) is an endoscopic procedure for imaging of the upper gastrointestinal tract (oesophagus, stomach, and duodenum), and the pancreas to biliary system (bile ducts, gallbladder, and pancreas) using a flexible endoscope equipped with a small specialized ultrasound probe.
An endoscopic ultrasound may be recommended to patients who have or are suspected to have pancreatic disease in the pancreas or bile duct and can be both a diagnostic and therapeutic procedure. Usually an endoscopic ultrasound is recommended after abnormal test results or a patient experiences worrying abdominal pain symptoms thought to be related to the pancreas or bile duct.
Common conditions that can be evaluated by EUS are:
1. gastrointestinal tract and pancreatic tumours,
2. submucosal tumours,
3. acute and chronic pancreatitis,
4. pseudocysts and
5. mediastinum lymph node.
Before undergoing EUS, patients are given sedation. A thin tube is inserted through the patient’s mouth and led down into the stomach. Once in the stomach, a small ultrasound probe at the tip of the tube emits soundwaves which produces a clear image of the desired area (such as the pancreas, digestive tract, or stomach). If masses or other signs of disease are found, a small biopsy will be taken for testing (with by EUS guided Fine Needle Aspiration (FNA).
Depending on the disease condition being evaluated, the duration of an endoscopic ultrasound examination usually lasts from 20 to 40 minutes.
A patient is asked to avoid eating and drinking for 8 hours before the procedure. Some medication should also be avoided prior to your appointment, so make sure to discuss this with your doctor. Following the procedure, it is advised that a family member or close friend should drive you home, that you avoid driving heavy machinery and signing important documents.
EUS is generally considered a safe procedure when performed by an expert health team. However, like most medical procedures it carries a small risk of complications.
Risks may include:
1. Tearing of the intestinal wall
2. Bleeding
3. Infection
4. Pancreatitis (only a risk if fine-needle aspiration (EUS-FNA) of the pancreas is done)
The cost of the procedure depends on whether one or more samples need to be taken for testing, or if it is simply an imaging procedure. Please contact our staff at 3946 6033 for further details.
Also feel free to check out our homepage for other bowel-related queries.


Related Information:
General Enquiry
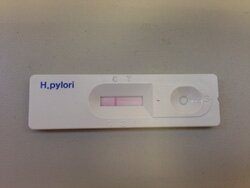
The urea breath test (UBT) is a non-invasive test for diagnosing the presence of a bacterium, Helicobacter pylori (H. pylori) in the stomach. H. pylori causes inflammation, ulcers, and atrophy of the stomach. The test also may be used for follow-up exam of H. pylori eradication treatment regime.
Comparing to OGD, urea breath test gives equally accurate result in terms of Helicobacter detection, while OGD provides additional information such as presence of inflammation or ulcer in the stomach.
Related Information:
General Enquiry
Helicobacter pylori Infection
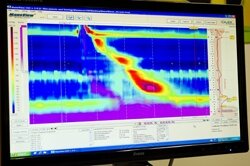
This test is indicated for suspected esophageal motility disorder (e.g. Achalasia), dysphagia, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain.
HRIM studies the function of lower esophageal sphincter (LES) and esophageal motility. Local anesthetic will be given to patient and a catheter of 3mm diameter will be intubated through the patient’s nostril into the esophagus. After 10 minutes of resting, a sequence of swallowing tests (salt water or sometimes solid food) will be performed to access the motility of esophagus.

Related Information:
General Enquiry
Gastroesophageal reflux disease
Indication: Gastroesophageal reflux disease (GERD) with poor response to acid suppressive therapy, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain
Procedure: The test studies the amount of acid reflux into the esophagus in 24 or 48 hours. Sedation will be given to the patient and a full diagnostic The Bravo capsule will be fixed to the esophagus with the help of endoscopy. The patient can be discharged after the procedure. The patient has to carry a wireless recorder during test (for 24 or 48 hours) and record the time of symptom onset, sleep and diet on a given diary. The patient will return the recorder and diary after 24 or 48 hours. The capsule will usually slough out spontaneously and passed out within 7-10 days. Compared to the traditional pH monitoring, Bravo wireless pH monitoring is more sensitive and better tolerated.

Related Information:
General Enquiry
Gastroesophageal reflux disease
This test is indicated for patients who have gastroesophageal reflux disease (GERD) with poor response to acid suppressive therapy, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain, liquid (acidic or non-acidic) regurgitation, repeated belching.
Local anesthetic will be given to patient and then a catheter of 1mm diameter will be intubated through the patient’s nostril into the esophagus. The patient will carry a portable recorder to which the catheter is connected. The patient can leave the hospital and resume normal activity during test, while recording the exact time of symptom onset, sleeping and diet on a given diary. The patient will come back to the hospital after 24 hours to have the catheter removed and to return the recorder and diary.

Related Information:
General Enquiry
Gastroesophageal reflux disease










